Ring chromosome 20. If you are a regular reader of this blog, you’ll know that much of our focus is on single genes and their relationships to neurodevelopmental disorder. Admittedly, we may neglect cytogenetic conditions. However, in today’s post, we highlight ring chromosome 20 as a likely underdiagnosed genetic epilepsy with distinct clinical features.
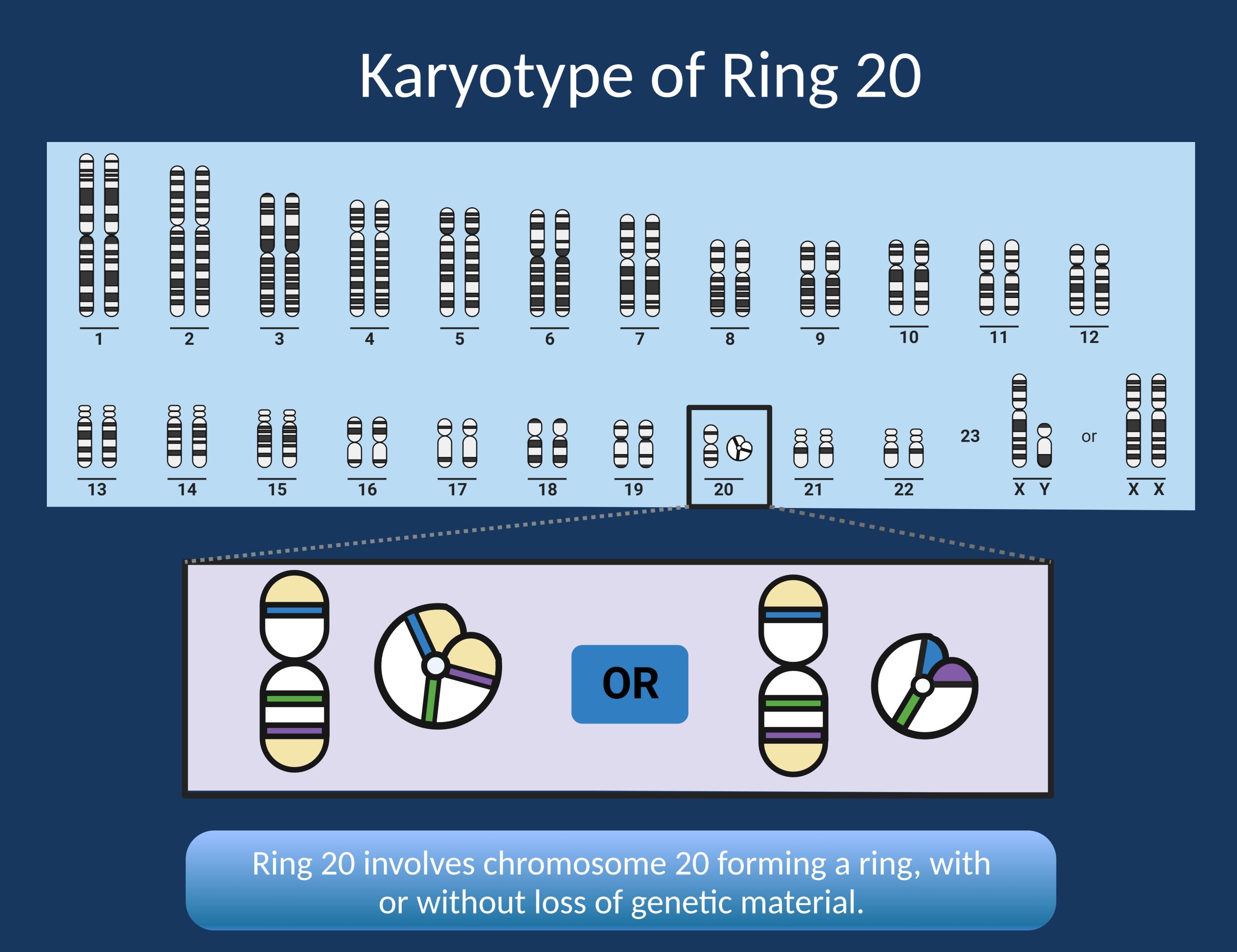
Figure 1. Ring chromosome 20 occurs when chromosome 20 forms a ring structure, with both ends connecting. This can result in no loss of genetic material or loss of genetic material from one or both ends of the chromosome. Karyotype is the only reliable way to make this genetic diagnosis.
1- Genetic testing methods. Cytogenetics is a foundational field in genetics and one that can admittedly be overlooked in an era where exome/genome sequencing are becoming the gold standard of clinical genetic testing. However, it is important to know the limitations of each genetic test in order to ensure that all differential diagnoses are detectable. In the case of ring chromosome 20, karyotype is the best diagnostic test. This is because next generation sequencing cannot detect structural rearrangements. Even chromosomal microarray cannot reliably detect ring chromosome 20. Because karyotype is not often considered in genetic testing for epilepsy, diagnosis of ring chromosome 20 is likely underdiagnosed.
2- Clinical features. Because ring chromosome 20 is likely underdiagnosed, it is important for clinicians to know the key features of the condition to identify when karyotype is needed in diagnostic evaluation. Some features that should raise suspicion for ring chromosome 20 include nonconvulsive status epilepticus and/or explosive onset epilepsy especially in a school age child.
3- More than the sum of its parts. There are several epilepsy genes on chromosome 20 that have been proposed to potentially explain the epilepsy phenotype in ring chromosome 20, particularly KCNQ2, DNAJC5, and CHRNA4. We know that chromosomal disorders are phenotypically distinct from their single gene constituents (PRRT2 in the recurrent 16p11.2 microdeletion is a prudent example), which is again demonstrated in this case as the epilepsy in ring chromosome 20 is distinct from the epilepsy genes it contains. However, this does not mean that the genes it contains should be discounted altogether. There is a case report of response to ezogabine, a potassium channel opener which is currently in clinical trial for treatment of KCNQ2-DEE, as an effective therapy in a child with mosaic ring chromosome 20. Still, much more systematic evaluation and evidence is needed to understand the relationship between ezogabine and seizures in ring chromosome 20.
Here is what you need to know. In 2023, we may often overlook cytogenetic conditions as a genetic cause of epilepsy. Exome/genome sequencing is at the forefront of genetic testing. However, not all genetic epilepsies can be detected using these methods, with ring chromosome 20 as a key example. We hope that this post will bring awareness to clinical indications for karyotype in people with epilepsy.

