In final week before our EuroEPINOMICS  bioinformatics workshop in Leuven people get a little busy and start reading up on all sorts of things. Accordingly, this week’s papers come from all areas of genetics and life science, including three studies in Annals of Neurology on epilepsy genetics.
bioinformatics workshop in Leuven people get a little busy and start reading up on all sorts of things. Accordingly, this week’s papers come from all areas of genetics and life science, including three studies in Annals of Neurology on epilepsy genetics.
Tag Archives: epilepsy research
A PhD in genomics – lessons learned
This is it! With finishing my PhD I have become an “adult” member of the scientific  community. I grew out of a bachelor in biochemistry on transfection methods in neuronal cell lines, a research semester in Canberra with focus on B-cell immunology and master into a PhD in epilepsy genomics. I was involved in the EPICURE IGE copy number projects and recently my work changed to the analysis of rare variants in RE and IGE in the EUROepinomics framework. During this time I was involved in the identification of variants in RBFOX genes and GRIN2A as well as other risk factors which are currently in review. I share my experience and thoughts and hope they help others who are about to or have just started their thesis. The aspects reflect my personal view and some are specific for graduation in disease genomics. Continue reading
community. I grew out of a bachelor in biochemistry on transfection methods in neuronal cell lines, a research semester in Canberra with focus on B-cell immunology and master into a PhD in epilepsy genomics. I was involved in the EPICURE IGE copy number projects and recently my work changed to the analysis of rare variants in RE and IGE in the EUROepinomics framework. During this time I was involved in the identification of variants in RBFOX genes and GRIN2A as well as other risk factors which are currently in review. I share my experience and thoughts and hope they help others who are about to or have just started their thesis. The aspects reflect my personal view and some are specific for graduation in disease genomics. Continue reading
Chutzpah, Zen and Fahrvernügen – the 2013 Sde Boker workshop
Desert Dessert. Cold temperatures, streets closed because of snow – this is not what you expect when traveling to Israel. You also do not expect to have the chance to taste traditional Bedouin food and to see a beautiful canyon every morning. The biggest surprise is that you do not expect this during a workshop. From Dec 12-15th, the European epilepsy genetic community gathered in Be’er Sheva and Sde Boker, Israel for a combined epilepsy genetics workshop and a Young Researcher Meeting. This is a brief attempt to capture the atmosphere of this workshop for everybody who could not attend. By the way, “desert dessert” is a port wine produced in the Negev desert.
The Hippocampus Conspiracy
Slightly misleading. The green and blue histological staining that has become the EuroEPINOMICS logo features a human hippocampus, a part of the human brain that is particularly important in human epilepsy. Temporal Lobe Epilepsy (TLE) is the most common epilepsy in adults and involves the hippocampal region. Ironically, TLE is the human epilepsy that has always been at odds with genetic research. Let’s review what we know about the genetics of TLE and “hippocampal genetics”. Continue reading
21st century digital boy: The Kiel Young Investigators’ Meeting
The children of the genomic revolution. There aren’t many possibilities for young researchers in epilepsy research to get together independently. Accordingly, we were in the fortunate position to host the first meeting for young researchers in pediatric epileptology in Kiel last week. I was asked by some participants to write a post on this. There were, however, two very specific instructions. First, I was asked to write about “Generations X and Y” and the resulting conflicts in science. Secondly, I was told not to write an ordinary meeting report, but something different… Continue reading
Epilepsy genes in noncoding RNA
Genome vs. exome sequencing. Can non-coding regions be skipped in the search for disease-causing variants? Is it worth to pay a higher price for sequencing the whole genome?
The sequencing company Complete Genomics (CGI) is already sounding the death knell for exome sequencing, arguing that the protein-coding genes cover only ~1% of the genome, while many loci identified by GWAS lie in the non-coding regions. CGI maintains that the price difference between whole-genome (WGS) and exome sequencing (ES) has become “less of an issue”. With declining sequencing prices, this will certainly be the case in the future – however, when multiplying the current added costs for WGS with the large numbers of cases and controls required for finding new hits in complex diseases, the proponents of ES have strong arguments. Will WGS explain more than the 10% expected for exome sequencing? Continue reading
Why CNS disorders are more likely to be monogenic
Once again, the flood of rare variants. Deep sequencing studies have revealed an unexpected plethora of rare variants, i.e. genetic variants that can only be found in few or even single individuals. While the genetic architecture of more common genetic variants, so-called Single Nucleotide Polymorphisms (SNPs) is well known through the HapMap project, the role of rare variants identified with recent sequencing studies is difficult to interpret. Basically, for an individual variant it is difficult to establish whether this variant is disease-causing or disease-related based on the frequency in cases. Establishing association at the same level of statistical significance as required for SNPs is difficult given that much larger samples are needed. Furthermore, protein prediction algorithms have their limitations and might not be able to discriminate an accidental from a causal variant, given that every individual might be homozygous or compound homozygous for gene-disrupting variants in at least three genes. We are drowning in a flood of rare variants and cannot distinguish pathological from benign variants very well yet. Continue reading
FAME – when phenotypes cross over but chromosomes don’t
Crompton and colleagues recently published the clinical and genetic description of a large family with Familial Adult Myoclonic Epilepsy (FAME). This phenotype is particularly interesting since it provides some insight into how neurologists conceptualize twitches and jerks. It is also a good example that large families do not necessarily result in a narrow linkage region, particularly when centromeric regions are involved.
What is myoclonus? Despite usually mentioned in the context of epilepsy, most people are inherently familiar with myoclonus. Most of us “twitch” when we fall asleep and sometimes experience this twitch as part of a dream. These episodes are entirely normal and are called hypnic jerks, but they give people a good idea of what a sudden, brief, shocklike, involuntary movement caused by muscular contraction or inhibition would feel like. Myoclonus in the setting of epilepsy is usually mentioned as part of a Juvenile Myoclonic Epilepsy (JME) or Progressive Myoclonus Epilepsy (PME). Please note that both epilepsies use different endings to describe the twitch (“-us” vs. “–ic”). This is mainly convention. Basically, myoclonus is a brief shock-like twitch, which can affect almost every part of the body and can be due to dysfunctions in various regions in the Central Nervous System.
The neuroanatomy of twitching. A motor command from the cerebral cortex has to pass through several steps prior to execution. For example, the simple command of tapping a finger on the table surface is prepared by the cortex through several loops before being sent down your spine. Accordingly, myoclonus can arise from different parts in the brain. (1) The cortical myoclonus is due to a purely cortical source and can be seen in many forms of symptomatic myoclonus. (2) The cortico-subcortical myoclonus is due to feedback from the cortex to other brain areas. This is the myoclonus we see in patients with JME. Both variants may be seen on EEG since the cortex is involved. (3) The subcortical-supraspinal myoclonus is generated in the brain stem or below and is responsible for phenomena such as hyperekplexia or startle disease. Some forms of hyperekplexia, literally “exaggerated surprise”, are due to mutations in genes involved in glycinergic transmission and can be found in some isolated communities such as the Jumping Frenchmen of Maine. (4) Finally, there is also spinal and peripheral myoclonus.
FAME – epilepsy or movement disorder? Familial Adult Myoclonic Epilepsy (FAME) is an enigmatic familial disorder with the triad of myoclonus, tremor and seizures. Several families have been described and two loci on 8q23.3-8q24.11 and 2p11.1-q212.2 for FAME have been established. The underlying genes are still unknown. Crompton and colleagues no describe a large six-generation family with FAME in Australia/New Zealand. The familial disease usually starts with tremor in early adulthood in the affected family members, even though a wide range of age of onset is observed. Interestingly, only a quarter of all affected family members had seizures, which is in contrast to previous studies. Therefore, FAME may actually be better characterized as a movement disorder with concomitant seizures rather than a familial epilepsy syndrome. The authors also point out the difficulties distinguishing FAME from the much more common essential tremor (ET). In particular, the well-described response to β-blockers seen in patients with ET can also be observed in some family members.

Figure 1. The candidate gene landscape of the chr2 FAME region. All genes were searched for the number of hits in PubMed for the listed search terms in an automated fashion. As usual in large linkage intervals, only few genes are known in the context of neurological disorders, while most genes are unknown.
The genetics of FAME. Crossovers during meiosis usually lead to a progressive narrowing of the linkage interval in familial disorders. However, the lack of crossover events leads to very large linkage intervals even in very extended families. The family described by Crompton et al. links to the pericentromeric region of chromosome 2. Pericentromeric regions usually have a low frequency of crossover events, and this phenomenon has also delayed the identification of other familial epilepsies such as Benign Familial Infantile Seizures with mutations in PRRT2. The linkage region contains almost 100 genes and Figure 1 shows the “candidate gene landscape” in this region. While some genes clearly classify as top candidate genes, the majority of the genes in this region are unknown in the context of epilepsy. Therefore, identification of the FAME gene will be exciting and provide us with novel insight on how genetic alterations may produce combined neurological phenotypes.
Be literate when the exome goes clinical
Exomes on Twitter. Two different trains of thoughts eventually prompted me to write this post. First, a report of a father identifying the mutation responsible for his son’s disease pretty much dominated the exome-related twittersphere. In Hunting down my son’s killer, Matt Might describes his family’s journey that finally led to the identification of the gene coding for N-Glycanase 1 as the cause of his son’s disease, West Syndrome with associated features such as liver problems. The exome sequencing that finally led to the discovery was part of a larger program on identifying the genetic basis of unknown, putatively genetic disorders reported in a paper by Anna Need and colleagues, which is available through open access. This paper is an interesting proof-of-principle study that exome sequencing is ready for prime time. Need and colleagues suggest exome sequencing can find causal mutations in up to 50% of patients. By the way, a gene also that turned up again was SCN2A in a patient with severe intellectual disability, developmental delay, infantile spasms, hypotonia and minor dysmorphisms. This represents a novel SCN2A-related phenotype, expanding the spectrum to severe epileptic encephalopathies.
The exome consult. My second experience last week was my first “exome consult”. A colleague asked me to look at a gene list of a patient to see whether any of the genes identified (there were 300+ genes) might be related to the patient’s epilepsy phenotype. Since I wasn’t sure how to best handle this, I tried to run an automated PubMed search for combination of 20 search terms with a small R script I wrote. Nothing really convincing came up except the realisation that this will be an issue that we will be increasingly faced in the future: working our way through exome dataset after the first “flush” of data analysis did not reveal convincing results. Two terms that came to my mind were bioinformatic literacy as something that we need to improve and Program or be Programmed, a book by Douglas Rushkoff on the “Ten commands of the Digital Age”. In his book, he basically points out that in the future, understanding rather than simply using IT will be crucial.
The cost of interpretation is rising. The Genome Center in Nijmegen suggests on their homepage that by the year 2020, whole-genome sequencing will be a standard tool in medical research. What this webpage does not say is that by 2020, 95% of the effort will not go into the technical aspects of data generation, but into data interpretation. For biotechnology, interpretation will be the largest marketing sector.

By 2020, probably more than 10 million genomes will have been sequenced. Data interpretation rather than data generation will represent the most pressing issue.
So, what about epilepsy? “50% of cases to be identified” sounds good for any grant proposal that I would write, but this might be a clear overestimate. Need and colleagues used a highly selected patient population and even in the variants they identified, causality is sometimes difficult to assess. We are maybe much further away from clinical exome sequencing in the epilepsies than we would like to admit. The only reference point we have for seizure disorders to date is large datasets for patients with autism and intellectual disability. While some genes with overlapping phenotypes can be identified, we would virtually be drowning in exome data without being capable of making sense of this.
10,000 exomes now. I would like to predict that after having identified some low-hanging fruits with monogenic disorders, 10,000 or more “epilepsy exomes” would have to be collected before making significant progress. It is, therefore, crucial not to be tempted by wishful thinking that particular epilepsy subtypes necessarily have to be monogenic, as in the case of epileptic encephalopathies or other severe epilepsies. Much of the genetic architecture of the epilepsies might be more complex than anticipated, requiring larger cohorts and unanticipated perseverance.
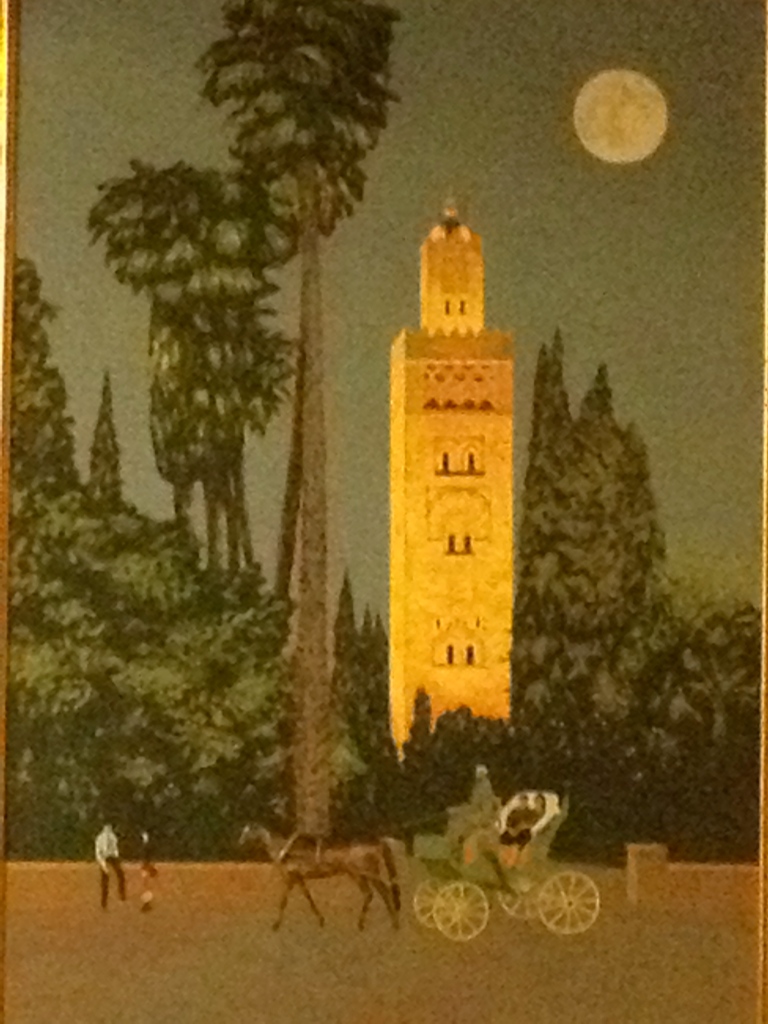
The Marrakesh diaries – DNA colonialism
A 21st century gold rush. Collections of biosamples, referred to as biobanks, are sometimes referred to as the ‘gold of the 21st century‘, as these collections will provide the key for translating the findings of biomedical research into patient treatments. The upcoming revolution of personalized health can only happen if well-curated patient samples for DNA, tissues and other biomaterials are available. In many European countries, large government-funded initiatives are on the way to build these collections. So far, so good.
DNA colonialism. But what does this have to do with colonialism? The phrase of DNA colonialism has a dual origin and was pretty much invented in parallel in a discussion I had with researches in Israel and Morocco. Given that this idea came up twice independently within a few weeks, it prompted me to put this together as a blog entry. DNA colonialism refers to the phenomenon that researchers from “developed” countries obtain valuable biosamples in “developing” countries for their research. Collaborations with emerging countries are becoming increasingly important given the particular genetic architecture in these countries, which lends itself to gene discovery. Often collaborating researchers in the emerging country are only involved on a very basic level and are sometimes not even involved in the final publication of the data. This phenomenon is frequently observed in the literature when the author list of novel gene findings in consanguineous families do not include researchers from the respective emerging country.
DNA mining leaves little behind other than empty mines. Within these bilateral collaborations, the genetic architecture of the “developing” countries is mined by Western researchers, which is sometimes interpreted as a modern form of colonialism. While there is little doubt that the findings originating from this research are important, there is little benefit for the emerging country. Examples where the gene findings in families are translated into screening programs are rare and -to my knowlegde- only exists for Bedouin population in the Southern part of Israel. Treatment options based on these findings are even rarer. Instances, in which a partnership between a “developing” and “developed” country has resulted in the creation of infrastructure on site are few.
New rules for “DNA trading”. What has to be done to avoid DNA colonialism and what would constitute a fair trade agreement to enable a productive partnership rather than an exploitation of the genetic architecture? Naturally, there is not a single definite solution for this issue, but at least two points may be raised in this context.
Biosamples are becoming more valuable. First, the relative value of biosamples in relation to genetic technologies is increasing. The price for Next Generation Sequencing technologies is constantly dropping and samples can be analyzed at much lower costs. This will naturally help the relationship between both partners as the effort to obtain sample is increasingly valued. Also, there is an increasing awareness regarding the IRB-related issues surrounding biosamples. While many researchers still feel that they lose the control over a given biosample once the sample leaves the country, the entire field is getting increasingly sensitized to these issues. Modern material transfer agreements might include well laid-out plans for what happens with samples once they cross international borders.
Redistribution, fostering intrinsic motivation. Secondly, research environments in developing countries would need to provide a commitment towards generating a sustainable infrastructure in emerging countries. Despite the naive impression that building good research environments is not possible in countries outside the Western sphere, there are examples that suggest otherwise. For example, the Kanaan lab in Bethlehem, Palestine, represents one of the of the premier labs worldwide for the research of genetic hearing loss and Dr. Kanaan has a strong commitment to establishing methods and technologies on site. As in many other instances, lack for funding for R&D is not a matter of resources, but of distribution. The question of to what extent pure external incentives such as large amounts of funding might help resolve these issues is uncertain, and one of the key challenges would be to foster intrinsic motivation for these issues in young researchers.
Implementing some of these issues might help researchers in emerging countries establish long-term plans to generate on-site know-how and infrastructure in order to fully participate as equal partners in international research networks. Eventually, the hunt for epilepsy genes does only start with the identification of these variants. If we ever have the hope that genetic findings in the epilepsies will impact on patient care and treatment, we as the EuroEPINOMICS consortium should strongly motivate our collaborative partners in emerging countries to be more than mere sample providers.