Telemedicine. Admittedly, this is a strange title for a blog post. This is a blog on epilepsy genetics, so why do we concern ourselves with telemedicine again? To make a long story short, telemedicine was the main avenue for outpatient child neurology care during the early phases of the pandemic. In the later phases of the pandemic, many centers have used a hybrid care model of in-person and telemedicine care. Evaluations for epilepsy genetics are more frequently performed via telemedicine than other child neurology indications, at least at some centers. Accordingly, for an epilepsy genetics team, understanding how well telemedicine works is highly relevant. Typically, scientific publications emphasize the successes of telemedicine. However, in a recent publication, we asked the opposite question: what happens when telemedicine does not work?
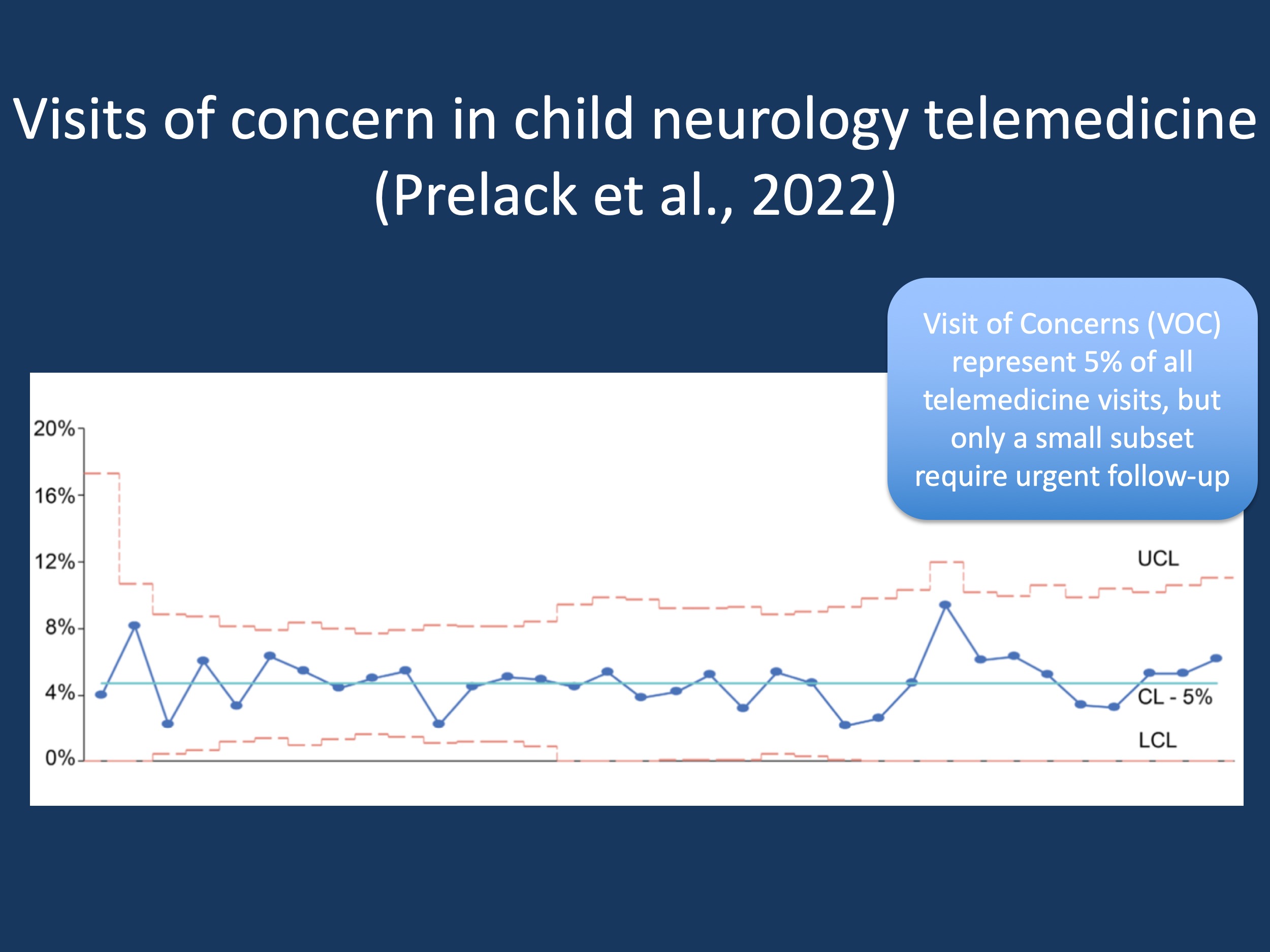
Figure 1. The frequency of Visits of Concern (VOCs) in child neurology telemedicine remained constant throughout the pandemic, accounting for 5% of all telemedicine visits. CL, center line (mean); UCL, upper control limit; LCL, lower control limit. Modified from Prelack et al., 2022.
VOC. In our recent publication by Prelack and collaborators, we took advantage of a new framework that we introduced during the onset of the pandemic – we embedded questionnaires within patient note templates that asked the question whether a telemedicine visit that was just performed necessitated in-person follow-up evaluation sooner than if the visit had been conducted in-person. In other words, we asked whether a telemedicine visit raised a concern with the provider that would not have been raised had the visit been performed in-person. Thus, the concept of the VOC was born, the Visit of Concern.
An example. I would like to use one case story during the pandemic as an example of a VOC. One of our providers was asked to see a new patient with a severe epilepsy during the early stages of the pandemic. The video connection with the family was somewhat shaky and the young child seemed to be obtunded – the provider was not able to truly assess the child’s mental status up to the point that they could reassure themselves that this was not potentially concerning, especially as they had not previously seen the patient. Had the evaluation been in-person, the provider could have performed a more detailed assessment, but this was not possible via telemedicine, compounded by the difficulties with the connection to the family’s device. The provider urgently admitted the patient for an evaluation. This case is an example of a VOC. But how often do VOCs occur and what factors are linked to them?
The 5% rule. Combining our analysis of Electronic Medical Records (EMR) and manual review, we assessed 7,130 telemedicine visits between March and November 2020. VOCs occurred in 5% of all visits (333/7,130). VOCs were more common when patients were younger, and patients with neuromuscular disorders and developmental delay had a higher proportion of VOCs than other neurological conditions. Demographic factors were associated with a higher risk of VOCs, including a lower household income or underrepresented minorities. However, demographic factors did not account for the majority of VOCs, nor did connectivity issues as in the case example above.
Telemedicine disparities. Our findings were different than our initial study by Rametta and collaborators where we initially did not find differences with respect to self-reported race in families participating in telemedicine care compared to prior in-person visits. It is important to note that disparities in telemedicine care were not limited to the initial stages of the pandemic but continue to exist. This is a call to action to generate more opportunities for underserved minorities to participate in telemedicine care, which many centers have already started to address.
Follow-up. We subsequently followed up on what happened to individuals where initial visits were flagged as VOCs. Most VOCs were benign and the provider simply suggested a sooner visit due to non-urgent issues. Direct action to ensure patient safety, such as urgent admission, only needed to be performed in 6% of all VOCs or 0.2% of all telemedicine visits. Accordingly, the case example mentioned above was only one out of 18 VOCs requiring urgent action within a total 10,502 telemedicine visits. This is reassuring and convincing evidence that the current practice of child neurology telemedicine is generally considered safe by providers. In our publication by Prelack and collaborators, we provide additional VOC case examples that demonstrate how providers have addressed particular VOC scenarios.
Concepts, concepts, concepts. Evaluating telemedicine visits may sound like a somewhat boring task, simply following and reporting trends within healthcare systems. However, this perception is incorrect. When our team was tasked with monitoring the telemedicine encounters, the first thing we needed to do was to be creative and invent novel concepts. I would like to give a shout-out to our telemedicine team at this point for being part of this creative process. Prior to the pandemic, concerning visits during in-person care were often not systematically captured. With the introduction of new technology during the COVID-19 pandemic, this suddenly became possible, opening up new ways to assess the quality of the care that our patient population is receiving.
What you need to know. Roughly 5% of all telemedicine visits in child neurology are concerning to providers, requiring in-person follow-up. However, only a very small subset of visits requires immediate follow-up such as direct admission to emergency rooms. Young age and developmental or neuromuscular conditions raise concerns more frequently that other clinical scenarios. In addition, the higher frequency of VOCs in underserved minorities emphasizes the important role of improving equitable access to telemedicine care.


