Disease burden. One aspect of neurodevelopmental disorders that we cover insufficiently on our blog is how epilepsy affects families. Not just the symptoms of seizures and developmental delay, but how the overall burden of developmental and epileptic encephalopathies (DEEs) affects the quality of life of patients. In a recent study, we took a first step towards measuring quality of life and assessing to what degree seizure control and quality of life in DEEs are related. To our surprise, we found that objective seizure control and quality of life are unrelated. In contrast, quality of life is related to a more nuanced measure, the number of days that were minimally disrupted by seizures.
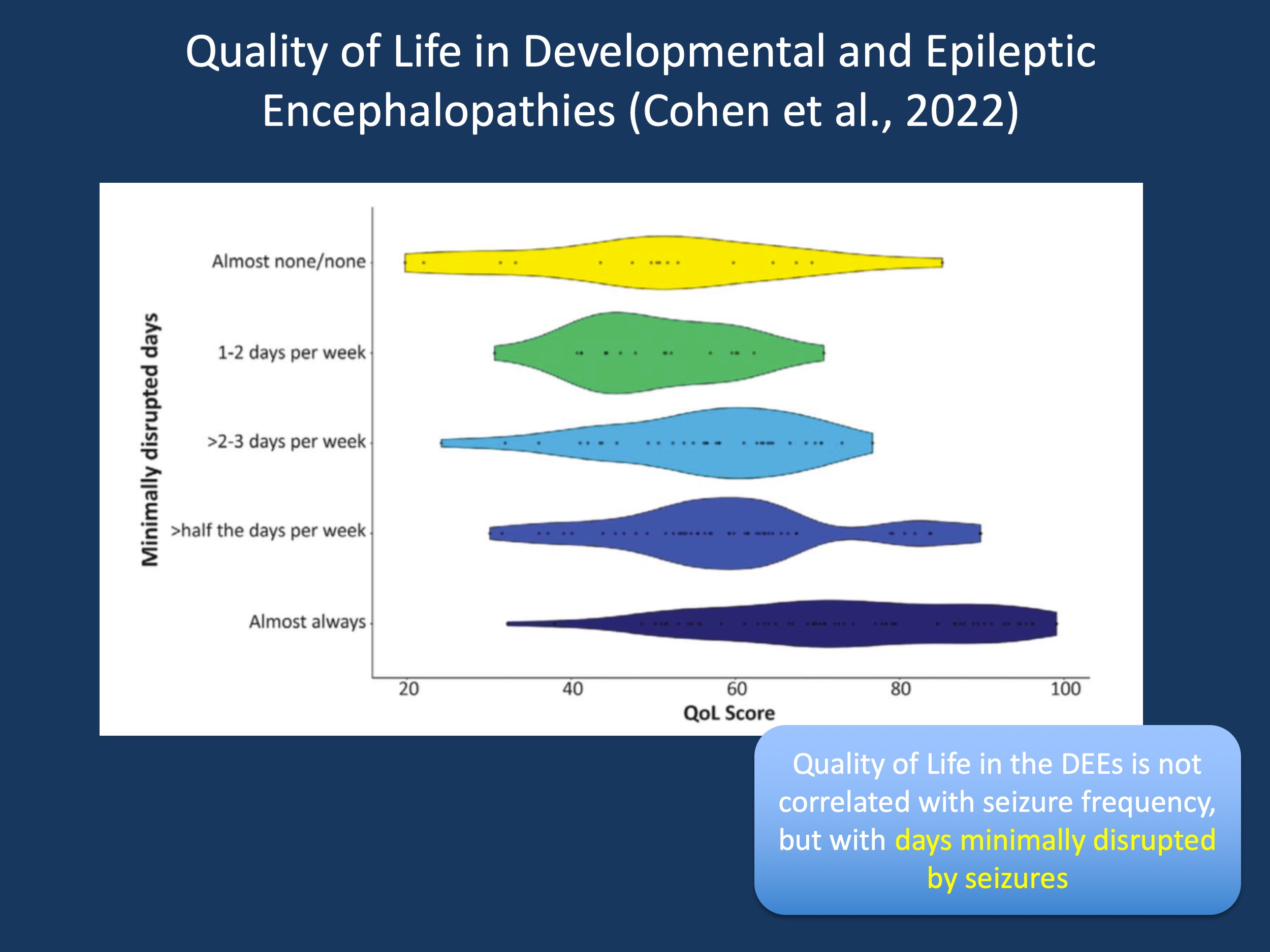
Figure 1. Relationship between quality of life (QoL) and (a) number of minimally disrupted days. Each dot represents a single participant’s response within the distribution of responses while the width of a given plot represents the probability of a given QoL score response using kernel density estimation. This finding might be relevant for future patient-centered outcome measures in precision medicine trials. Quality of life in the developmental and epileptic encephalopathy itself may be insufficient to account for the impact of seizures. However, a “hybrid” measure such as quantifying the disruption caused by seizures may represent a measurement that captures elements of quality of life and seizures (Cohen et al., 2022).
Questionnaire. Our study, published in DMCN with our ENGIN Genetic Counselor Stacey Cohen as the first author, assessed 89 questionnaire items that were distributed to families of individuals with genetic DEEs through advocacy organizations, with SCN2A (n=42/173, 24%), SLC6A1 (n=28/173, 16%), SCN1A (n=22/173, 13%), and KCNQ2 (n=21/173, 12%) representing the most common genetic diagnosis. Our questionnaire included items regarding clinical features such as seizures frequency, demographics, and quality of life (QoL), using items from existing validated questionnaires. We summarized QoL across different domains, such as social interaction and physical health, as a composite score to have a single number that we could analyze across the entire group. Here are five findings of our study that we found interesting and that may help us design better outcome measures for the DEEs.
1 – We can measure QoL in DEEs
Our blog is a neurogenetics blog where we typically discuss genetic etiologies and “hard facts”. Quality of life, at first glance, may seem somewhat fuzzy, subjective, and hard to track and compare. These assumptions are somewhat outdated and incorrect. Over the last two decades, effort has gone into developing standardized, valid tools with established construct, content, and face validity. One of these tests is the Quality of Life Inventory-Disability (QI-Disability), which has been shown to be a valid measure across the spectrum of intellectual disability and neurodevelopmental disorders. In brief, QoL is not just a difficult-to-grasp concept relating to personal well-being, but a feature of living with a disease that can be measured, tracked over time, and compared.
2 – Seizure frequency is unrelated to QoL
We had 141 participants with QoL scores and seizure frequency responses reported by their caregivers. First, we did not find significant difference in QoL scores between individuals with seizures and individuals who were seizure free for at least a year (p=0.14). There was also no significant difference in QoL score between participants who never had seizures and individuals with a history of seizures with at least 1 day of seizure freedom (p=0.41). In brief, we did not find a clear correlation between seizure frequency and QoL. Whether this finding is surprising or trivial for you likely depends on your experience with DEEs. In clinical practice, we often see that comorbidities, rather than the actual seizure frequency, are the main drivers of disease burden, especially in individuals with frequent, ongoing seizures. This finding reflects our clinical experience and emphasizes the role of non-seizure outcomes and caregiver perception of symptoms. However, this should not de-emphasize the importance of seizure reduction or seizure freedom as a treatment goal. The risk for seizure-related injury and seizure-related mortality is related to the presence of seizures and seizure frequency. This potentially creates a conflict with treatment decisions to increase QoL, such as accepting a baseline seizure frequency to prevent sedation from additional medications, which might not be the same treatment strategies to minimize the risk for seizure-related injury and mortality.
3 – Frequency of days disrupted by seizures is associated with QoL
Despite the fact that seizure frequency itself is not directly related to quality of life, seizures still play a major role in determining how DEEs impact families and caregivers. However, the connection between these issues is not objective seizure frequency, but the way that seizures disrupt the day-to-day life of families and caregivers. For example, we found that a difference between participants experiencing minimally disrupted days for the majority of the month compared to participants with minimally disrupted days for the minority of the month, accounted for almost 20% of the QoL score. When we used other methods to assess the relationship between quality of life and the disruptive effect of seizures on daily life, we found comparable results. This highlights an interesting feature that might be relevant for future patient-centered outcome measures. Quality of life in the developmental and epileptic encephalopathies itself may be insufficient to account for the impact of seizures. However, a “hybrid” measure such as quantifying the disruption caused by seizures may represent a measurement that captures elements of quality of life and seizures.
4 – Individuals with DEE have lower QoL scores than other neurodevelopmental disorders
Using the QI-Disability allowed us to compare our results with assessments in other neurodevelopmental disorders such as Rett Syndrome, cerebral palsy, and Down Syndrome. We found that the QoL scores in developmental and epileptic encephalopathies were almost 10% lower. While there are many factors that may account for this, we speculate that this difference may be due to the additional impact of seizures, particularly early-onset, intractable seizures. This clearly highlights the overall burden of disease in DEEs and to what degree this affects families. Interpreting the data in a different way, we could show that, despite the lower scores in the DEEs, the scores across a range of neurodevelopmental disorders are comparable, adding additional validity to these tools.
5 – QoL is not static, but depends on community factors and medication side effects
One important feature to emphasize is that QoL is not a fixed value that is only determined by the disease itself. The quality of life of an individual with DEE may vary due to a variety of factors. The only demographic factor that we could identify was an approximate 20% difference between families living in urban and rural areas. Families living in rural areas reported lower QoL scores, which emphasize the challenges of providing health care for rare disease in communities outside the major metropolitan areas where healthcare options may be somewhat limited, adding to the burden to the family. On a larger scale, it emphasizes that community factors clearly play a role in how the burden of disease in the genetic epilepsies impacts families. In addition to the impact of community factors, we also found an almost 25% difference in QoL due to medication side effects and a strong effect of the total number of medical diagnoses, especially when individuals had more than 10 diagnoses.
What you need to know.
Stacey’s study was our first step towards measuring patient-reported outcome measures, trying to understand the unique situation in the DEEs where both seizures and the burden of complex neurodevelopmental disorders impacts on the quality of life. We find that seizure frequency itself is not correlated to quality of life, but that there are other seizure-related measures that are highly correlated, such as the disruptive effect of seizures on daily life. This emphasizes the need to address disease severity in DEEs holistically to inform patient care and outcome measures in future precision medicine trials.


